Shoulder Replacement Commonly Asked Questions
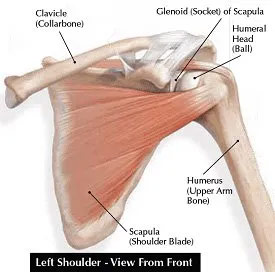
The shoulder joint is very complex and involves three bones and more than one joint. These bones are the clavicle (collar bone), the scapula (shoulder blade), and the humerus (upper arm bone). Numerous muscles, ligaments, and tendons surround the joint (Figure). The upper end of the arm bone (humerus) and the outside edge of the scapula bone (glenoid) form a “ball-and-socket joint.” This joint is remarkable because it typically allows greater range of motion than any other joint in your body.
Shoulder replacement surgery is most commonly used for severe degenerative joint disease (osteoarthritis) of the ball-and-socket joint. When the smooth surfaces (cartilage) of the ball and socket become rough, they rub against each other rather than glide. This rubbing causes pain, stiffness and swelling. Most patients who decide to have shoulder replacement surgery have experienced shoulder pain for a long time. Many patients have developed pain that limits their daily activities, as well as interferes with their sleep. Shoulder stiffness also interferes with the use of their arm for everyday activities. A shoulder replacement is performed to alleviate shoulder pain. It also helps to improve the range of motion of your shoulder joint, which also improves your function and the quality of your life.
The two most common types of shoulder replacement are an anatomic shoulder replacement and a reverse total shoulder replacement.
With an anatomic total shoulder replacement, the ball (humeral head) of the shoulder joint is replaced with an implant that includes a stem with a smooth, rounded metal head. The socket (glenoid) is replaced with a smooth, specialized plastic that is cemented into place. In essence the diseased cartilage is removed and resurfaced with the two components (Figure 2). In some cases, just the ball is replaced, which is called a partial replacement or hemiarthroplasty.
With a reversed total shoulder replacement, the normal structure of the shoulder is “reversed.” The ball portion of the implant is attached to the scapula (where the socket normally is) and the artificial socket is attached to the humeral head (where the ball normally is) (Figure 3). This allows the stronger deltoid muscles of the shoulder to take over much of the work of moving the shoulder, increasing joint stability. A reversed procedure is use for patients with a severely torn and compromised rotator cuff. It is also commonly used in revision surgery cases.

In most cases shoulder replacement is very successful. Typically, patients gain 50 degrees in forward elevation (raising the arm straight ahead). In other words, most patients go from raising their arm at or below shoulder level to being able to raise the arm above the shoulder. Similarly, rotation out to the side improves on average by 30 degrees. Rotation behind the back also improves. The survival of the implant is 90 to 95% at 10 years after surgery and approximately 80% 20 years after surgery.1-4
In partial replacements only the ball or just a portion of the ball is replaced. Sometimes this is called a resurfacing. A partial replacement can be successful in select cases depending on patient age and the quality of the glenoid. However, the vast majority of patients will have a better outcome with a total shoulder replacement. Study after study has demonstrated that in most cases a total shoulder replacement leads to improved motion, less pain, and less need for repeat surgery compared to a partial replacement.1,2,5,6 This makes sense since arthritis affects both sides of the joint (the ball and socket). Additionally, the approach to the shoulder joint requires the same incision whether a partial or complete replacement is used.
Most people know someone who has had a hip or knee replacement. Knee replacement is the most common replacement performed in the US each year. Hip is the next most common and shoulder is the 3rd most common. The results of shoulder replacement are similar to hip and knee replacement. Studies have also shown that the complication rate is lower with a shoulder replacement compared to hip and knee replacement.7
As with any surgery, there is always a risk of complications. Infection and glenoid (socket) component failure are the most common complications in shoulder replacement. This risk of complication that affects outcome is roughly 5% for an anatomic shoulder replacement. Infection is about 1-2%. For reverse shoulder replacements the complication rate is higher and is 10-20% and includes infection, component failure, acromion stress fracture, and dislocation. The need for a blood transfusion after shoulder replacement surgery is very low at less than 5%.8-10
Most shoulder replacements are performed by surgeons who perform less than 10 replacements a year.11 Multiple studies, however, have shown that complication rates are lower in the hands of an experienced surgeon, performing the surgery in a high-volume hospital.12-14 Patients are encouraged to choose a qualified surgeon with focused experience in shoulder procedures. Surgeons who perform a higher volume of shoulder replacements each year bring added expertise and consistency to the procedure.
Shoulder replacement is performed in the hospital with the help of an experienced, specialized surgical team. The procedure generally takes 2 hours. Afterwards, patients stay in the hospital overnight. Many patients are able to go home the day after surgery. In some cases, particular for people who do not have assistance at home, a longer hospital stay is required and a brief stay in a skilled nursing facility may be necessary for additional assistance. To get to the shoulder joint an incision is made on the front of your shoulder. After exposing the shoulder joint, the damaged ends of the bone (humerus and glenoid) are removed. The bone is prepared for the replacement with the artificial joint. The artificial joint is made of metal, usually a titanium or a cobalt-chrome alloy. For a standard shoulder replacement, the stem is placed inside the humerus bone, usually without cement using a “press-fit” technique. The glenoid component is made of a special plastic (polyethylene). The glenoid is cemented into place. Not all patients require a glenoid component and the final decision to use a glenoid component is made during the surgery. For reverse shoulder replacements the ball is secured to the socket with a press-fit and supplemented with screws. The humeral stem is then press-fit or cemented into place. A high-strength plastic then is placed to act as a spacer between the stem and the ball.
Most people are able to return to normal everyday activities such as dressing themselves and grooming within the first two weeks after successful shoulder replacement surgery. It is good to have someone who can help with daily activities for the first couple of weeks after surgery.
In most cases your surgical incision will be closed with absorbable sutures and covered with surgical glue. In that case you may shower 2 days after surgery. Water can pass over the wound, but please do not soak in a pool or hot tub until 2 weeks after surgery. To wash under your armpit, lean over and dangle the arm at the side. After a couple of days, a bandage is not needed. If the incision is closed with staples, showering may occur 3 days after surgery and a bandage should cover the incision until the 2-week follow-up.
You cannot drive while taking narcotic pain medication. Legally, your provider must recommend that you delay driving until you are out of your sling. This is for 4 to 6 weeks depending on the type of shoulder replacement surgery. Standard total shoulder replacements and partial replacements require a sling for 4 weeks after surgery. Reverse total shoulder replacements require a sling for 6 weeks.
Return to work will be dictated by your type of work and your desire to return. Most commonly, you will be advised to take at least 2 weeks off of work. Some patients wish to return earlier, but it is better to plan for more time off and return early then vice versa. Immediately after surgery you can move your elbow and wrist up and down. This allows you to eat, drink, write, use a keyboard and do other minimal activities that do not require the use of your shoulder.
Most people return to all of their normal activities after shoulder replacement. In fact, many patients are able to do more because their motion is improved and their pain is decreased. Activities that involve a significant lifting or accelerate the arm (golf, tennis) are allowed 6 months after surgery. While there is no consensus among shoulder experts, in general it is recommended that you do not frequently lift over 25 pounds after a shoulder replacement. This is not to say that is cannot be done occasionally (like for lifting a suitcase). But, if someone does frequent lifting, particularly at or above shoulder level, the prosthesis is more likely to wear out.
Shoulder replacements do contain metal, so this is a possibility, but it depends on the sensitivity of the detector and the amount of other metal in your body/on your clothes. If you do set off the detector, you simply will need a manual scan. We do not provide cards stating that you have a joint replacement since these are not accepted by the TSA.
Guidelines will vary by provider. Your provider may prescribe antibiotics or recommend waiting at least 3 months after shoulder replacement to have dental work.
References
1. Bryant D, Litchfield R, Sandow M, Gartsman GM, Guyatt G, Kirkley A. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am 2005;87:1947-56.
2. Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am 2000;82:26-34.
3. Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: analysis of 2588 shoulders over three decades (1976 to 2008). J Bone Joint Surg Br 2011;93:1513-7.
4. Walch G, Young AA, Melis B, Gazielly D, Loew M, Boileau P. Results of a convex-back cemented keeled glenoid component in primary osteoarthritis: multicenter study with a follow-up greater than 5 years. J Shoulder Elbow Surg 2011;20:385-94.
5. Edwards TB, Kadakia NR, Boulahia A, Kempf JF, Boileau P, Nemoz C et al. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: results of a multicenter study. J Shoulder Elbow Surg 2003;12:207-13.
6. Radnay CS, Setter KJ, Chambers L, Levine WN, Bigliani LU, Ahmad CS. Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: a systematic review. J Shoulder Elbow Surg 2007;16:396-402.
7. Farmer KW, Hammond JW, Queale WS, Keyurapan E, McFarland EG. Shoulder arthroplasty versus hip and knee arthroplasties: a comparison of outcomes. Clin Orthop Relat Res 2007;455:183-9.
8. Cheung EV, Sperling JW, Cofield RH. Revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg 2008;17:371-5.
9. Sperling JW, Hawkins RJ, Walch G, Mahoney AP, Zuckerman JD. Complications in total shoulder arthroplasty. Instr Course Lect 2013;62:135-41.
10. Bohsali KI, Wirth MA, Rockwood CA, Jr. Complications of total shoulder arthroplasty. J Bone Joint Surg Am 2006;88:2279-92.
11. Hasan SS, Leith JM, Smith KL, Matsen FA, 3rd. The distribution of shoulder replacement among surgeons and hospitals is significantly different than that of hip or knee replacement. J Shoulder Elbow Surg 2003;12:164-9.
12. Sherman SL, Lyman S, Koulouvaris P, Willis A, Marx RG. Risk factors for readmission and revision surgery following rotator cuff repair. Clin Orthop Relat Res 2008;466:608-13.
13. Jain N, Pietrobon R, Hocker S, Guller U, Shankar A, Higgins LD. The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am 2004;86-A:496-505.
14. Hammond JW, Queale WS, Kim TK, McFarland EG. Surgeon experience and clinical and economic outcomes for shoulder arthroplasty. J Bone Joint Surg Am 2003;85-A:2318-24.